
Patient Information
Growth & Growth Disorders
GROWTH ASSESSMENT / GROWTH DISORDERS
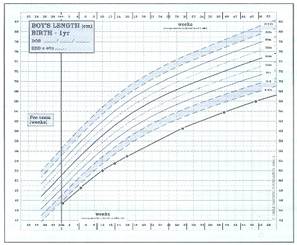
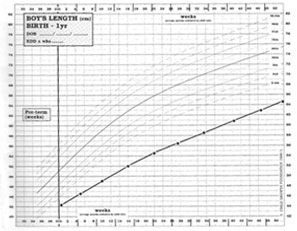
| Weight : | birth 2, 4, 6, 8, 12, 16 weeks, 6-8 months, 1 year. |
| Length : | 10 days and 3 monthly up to year 1. |
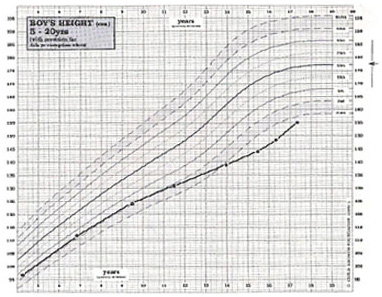
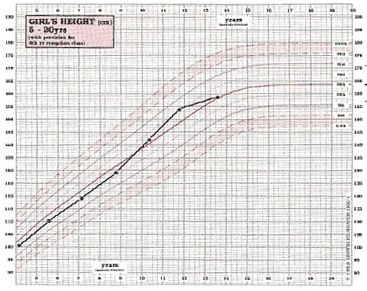
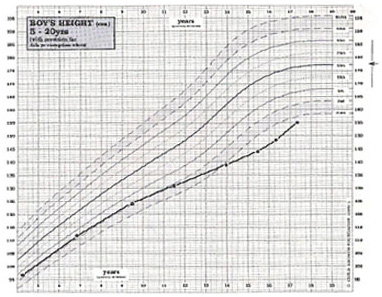
| Height : | Yearly from 18 months, school entry and routine checks at school. |
| Head Circumference : | 36 hours, 10 days and 8 weeks and as indicated. |
If there is any concern about growth, measurements should be taken more frequently.
Record child’s measurement and plot on growth charts
| Is this child small/tall but appropriate for parental heights? | Yes | Normal short/tall stature |
| Is child inappropriately short/tall for parental heights? | Yes | Refer to Paed Endocrinologist |
| Is child growing at an inappropriate growth rate? |
Possible Diagnosis
| Small for chronological age | GROWTH DELAY |
| Abnormal karyo type | CHROMOSOME ABNORMALITIES • Turner Syndrome • Down’s Syndrome |
| Low brithweight, thin, dysmorphic, possible asymmetry | INTRAUTERINE GROWTH RETARDATION (IUGR) • Including Russel Silver syndrome |
| Dysmorphic, cardiac problems | NOONAN SYNDROME |
| Abnormal hypopituitary function | ENDOCRINE DISORDERS • Growth hormone insufficiency • Panhypopituitarism • Hypothyroidism • Cushing's Syndrome • Premature sexual Maturation • Environmental growth failure |
| Dysmorphic | BONE DYSPLASIAS • Achondroplasia • Hypochondroplasia |
| Chronic ill health | CHRONIC DISEASES • Congenital heart disease • Renal failure • Coeliac/Crohn’s disease • Cystic Fibrosis • Asthma / eczema |
| Inappropriate tall stature | SYNDROMES • Marfan • Sotos • Klinefelter’s ENDOCRINE • Precocious puberty |
NORMAL GENETIC SHORT/TALL STATURE
 All children who are considered short/tall should be assessed for their MPC and TCR (see page 5). If their height is within normal limits for their parents and they are growing at a normal rate, they are normal, whatever their position within the population standards.
All children who are considered short/tall should be assessed for their MPC and TCR (see page 5). If their height is within normal limits for their parents and they are growing at a normal rate, they are normal, whatever their position within the population standards.
There is no effective treatment for genetic short stature. The availability of biosynthetic growth hormone has allowed increased interest in the use of this substance for the treatment of children who are very short. This is still in the stage of clinical trials but available evidence suggests that final stature will not be altered significantly. While it is clear that even in children with normal growth hormone secretion, a short-term acceleration in growth may be achieved during growth hormone therapy, there is no certainty at this time that the long-term final height prognosis is altered. Further careful studies, extending over a number of years, will be necessary to show this. However, in the USA, there is a much more liberal treatment regimen for children with genetic short stature. Although this probably represents a very heterogeneous group of children, growth hormone is now licensed for use in this indication.
CONSTITUTIONAL DELAY/ADVANCEMENT OF GROWTH AND PUBERTY
Constitutional delay of growth in puberty (CGDP) frequently causes concern and seems to be more prevalent in boys than girls. It is often first noticed when the boy seems to have stopped growing, has younger siblings catching up or even being taller than him, or has classmates leaving hi behind. Growth delay of up to two years is not uncommon and a small number of children are delayed three, or even four years. Frequently one of the parents, an aunt or an uncle, brother or sister, will have had growth delay. A mother will often be able to establish that she was 15 or more years old at menarche instead of the more usual 12 to 14 years : it may be more difficult to establish a father’s pubertal delay owing to the lack of a fixed event such as menarche.
Once growth delay has been established any boy or girl can be absolutely reassured that puberty occurs in the end and that they will develop quite normally in every way. They can be reassured with a full demonstration of facts, figures, charts and predictions. Children find the information that they are simply taking after their mothers or fathers reassuring if not particularly welcome. What reassurance does not do is remove the very real physical handicap associated with being small and, worse, remaining pre-pubertal with a peer group of adolescents.
GROWTH ASSESSMENT / GROWTH DISORDERS
(A GUIDE FOR PARENTS AND PATIENTS)
Once the diagnosis is established, there is little to do but separate such children from the adverse environment. Away from home, even in hospital where the reversibility of hypopituitarism can be demonstrated, the catch-up growth is usually spectacular being as good as that of a growth hormone deficient child who is given growth hormone replacement therapy.
There are lesser degrees of this problem in which children grow at a sub-optimal rate when in a disturbed environment. It is not unusual to see “spontaneous” catch up growth in a short child after a period of time (i.e. if parents separate or if there has been a move of home or school.
INTRAUTERINE GROWTH RETARDATION / RUSSELL SILVER SYNDROME
Diagnosis : Majority of cases should be diagnosed by age 2
Treatment : GH approved for treatment from the age of four years
Under-development of a baby in utero may be due to a problem with the fertilized ovum, the placenta that limits the supply of foods and oxygen to the fetus, or to disease or malnutrition in the mother. Certain of the first, and all of the second and third types of problem lead to poor growth of the baby and hence lead to a small size at birth. This smallness of size may be known only through weight. Though length would often be more informative, it is unfortunately not routinely measured in hospitals in India, although accurate apparatus for measuring length now exists.
Standards for birth weight and length are available for each week of gestational age; the centiles are different for girls and boys and for first-born and later-born. We are concerned here only with small-for-dates babies i.e. those who are below the centile limits for weight at their particular gestational age.
Babies who are simply born early, i.e. more than 32 weeks, and who are at the normal weight for that length of gestation, usually catch up to a perfectly normal height. Studies are currently ongoing to assess growth and “Catch-up” in very premature babies (i.e. <32 weeks gestational age). Indeed ‘catch-up’ growth may occur up to the age of six years, although more usually this commences during the first year of life. Small-for-dates babies may be born at term, or may be born after a shorter gestational period.
Russell Silver Syndrome
The majority of small-for-dates children, particularly those born at term, grow within the normal centiles. However, they do not fulfit their genetic potential and so are often small for their parents’ heights. Their average height centile seems to be about the 2nd. Others, however, fail to catch up in this way. They remain very short, lack subcutaneous fat and have a characteristic facial appearance. The face as a whole is triangular, with large eyes and small lower jaw; the forehead is large and prominent in relation to the face, and the ears are set low in the head and tend to stick out. The bridge of the nose is usually depressed and the mouth turned down at the corners. A proportion of these children have marked asymmetry of the limbs or body, one arm or leg being longer than the other, or one side of the face or chest more developed. The condition constitutes a specific syndrome known by the name Russell Silver after the two pediatricians who independently described it in the 1950s. Educational development often requires extra help.
 It is very important to provide calorie supplements and usually a more aggressive approach for calorie supplements may require gastrostomy tube. Children with Russell Silver syndrome commonly have reduced calorie intake for several reasons, including a high-arched palate, decreased appetite and gut dysmotility. It is very important to involve the opinion of a paediatric gastroenterologist at an early stage. Growth hormone treatment is now licensed for short children with intrauterine growth retardation/Russell Silver syndrome, but only from 2 years in USA & 4 years in UK. Growth hormone treatment not only improves the short-term growth rate, but also improves final height attainment. There may also be important benefits by improving blood sugar control (see below). These children are healthy and active, though usually very thin but should not be regarded as delicate. In middle childhood they put on some subcutaneous fat and their puberty occurs at a slightly earlier time but in the normal sequence. The syndrome hardly ever occurs twice in the same family, so the mother of such a child can be reassured about the subsequent pregnancies.
It is very important to provide calorie supplements and usually a more aggressive approach for calorie supplements may require gastrostomy tube. Children with Russell Silver syndrome commonly have reduced calorie intake for several reasons, including a high-arched palate, decreased appetite and gut dysmotility. It is very important to involve the opinion of a paediatric gastroenterologist at an early stage. Growth hormone treatment is now licensed for short children with intrauterine growth retardation/Russell Silver syndrome, but only from 2 years in USA & 4 years in UK. Growth hormone treatment not only improves the short-term growth rate, but also improves final height attainment. There may also be important benefits by improving blood sugar control (see below). These children are healthy and active, though usually very thin but should not be regarded as delicate. In middle childhood they put on some subcutaneous fat and their puberty occurs at a slightly earlier time but in the normal sequence. The syndrome hardly ever occurs twice in the same family, so the mother of such a child can be reassured about the subsequent pregnancies.
The cause of the disorder is unknown, although in a small proportion of mildly affected children there is a chromosomal abnormality. The prognosis may be improved by the treatment given to low birth weight babies nowadays, which consists of feeding them more intensively than before. This may also be important in the prevention of hypoglycaemia (low level of sugar in blood) which is more common in these babies.
Achondroplasia
GROWTH ASSESSMENT / GROWTH DISORDERS
(A GUIDE FOR PARENTS AND PATIENTS)
CARTILAGE AND BONE DISORDERS
Diagnosis : Majority at birth by radiological examination
Treatment : Usually surgical limb lengthening, GH in trials
There are a large number of bone disorders that affect growth; they are mostly rare and many are inhertited. They are known as skeletal dysplasias and the best known is achondroplasia.
 Children and adults with achondroplasia have short upper arms and thighs, a normal length back, a large head, and a characteristic face with depressed nasal bridge, small nose and large forehead. They appear to have large muscles for their leg length. They are of normal intelligence and health. Achondroplasia is caused by a mutation of a single gene and has a dominant pattern of inheritance. This means that, on average, half the children of a parent with achondroplasia will be affected. In most cases, however, there is a new mutation, without any family history and it seems that this particular gene is one of the most unstable in the human complex.
Children and adults with achondroplasia have short upper arms and thighs, a normal length back, a large head, and a characteristic face with depressed nasal bridge, small nose and large forehead. They appear to have large muscles for their leg length. They are of normal intelligence and health. Achondroplasia is caused by a mutation of a single gene and has a dominant pattern of inheritance. This means that, on average, half the children of a parent with achondroplasia will be affected. In most cases, however, there is a new mutation, without any family history and it seems that this particular gene is one of the most unstable in the human complex.
At present, treatment depends primarily on new surgical techniques of limb lengthening. Growth hormone treatment may improve short-term growth rate, especially if started at an early age. However, it is not yet known whether this improves final height and growth hormone use in this condition is therefore still being evaluated through clinical trials.
Hypochondroplasia
This is a similar syndrome to achondroplasia but the physical characteristics and short stature are less marked. Like achondroplasia, the short legs are responsible for the short stature. The face is normal (though it has some tell tale features to the experienced eye) and children with hypochondroplasia often may be diagnosed as being very short normal’s. Hypochondroplasia is also inherited as a dominant gene, but seems to be separate from the achondroplasia gene; the two condition very seldom appear in the same family. In hypochondroplasia, one of the parents frequently has the disorder.
There is no certain way of confirming what is sometimes a difficult diagnosis. The most helpful feature is comparison of sitting-height and leg-length centiles. While in achondroplasia the X-ray signs are marked and characteristic, in hypochondroplasia they are minimal. The effect growth hormone treatment is being evaluated through clinical trials.
Other Skeletal Dysplasias
There are over one hundred such conditions of which achondroplasia and hypochondroplasia are two of the most common. Other bone disorders are more rare; some affect limbs only, some the trunk and some both. To date, none have any specific treatment although surgical limb lengthening is potentially the most promising, while the use of growth hormone is being evaluated through clinical trials.
Growth Hormone Deficiency
GROWTH ASSESSMENT / GROWTH DISORDERS
(A GUIDE FOR PARENTS AND PATIENTS)
 If reassurance does not completely satisfy the patient then there are, at present, two options for treatment. When the anxiety only concerns height, the first line of treatment is the mild anabolic steroid, oxandrolone. This makes no difference to final height but it does initiate the growth spurt a little earlier than would occur with no treatment. If a boy is also concerned about his lack of pubertal development then testosterone, the male sex hormone, can be used. In girls, low dose estrogen can be used. It should be emphasized that these forms of therapy require careful monitoring by specialists experienced in the treatment of growth problems.
If reassurance does not completely satisfy the patient then there are, at present, two options for treatment. When the anxiety only concerns height, the first line of treatment is the mild anabolic steroid, oxandrolone. This makes no difference to final height but it does initiate the growth spurt a little earlier than would occur with no treatment. If a boy is also concerned about his lack of pubertal development then testosterone, the male sex hormone, can be used. In girls, low dose estrogen can be used. It should be emphasized that these forms of therapy require careful monitoring by specialists experienced in the treatment of growth problems.
Constitutional advanced growth is the converse of growth delay but rarely presents as a clinical problem
ENDOCRINE GLAND DISORDERS
The two main endocrine disorders that cause short stature are growth hormone deficiency and thyroid deficiency.
Diagnosis : If MPHD (see below) at birth. If solely GHD possible by 18 months. 80% of cases of GHD should be diagnosed by school entry.
Treatment : Growth hormone (GH) replacement therapy.
Growth Hormone Deficiency (GHD) is generally due to the pituitary gland being unable to produce sufficient GH to generate the growth process. GHD does not affect intrauterine growth, at least to an extent measurable by birth weight or length, but from the second year of life growth is slower than normal and occasionally growth failure commences from birth. Most cases of growth hormone deficiency are idiopathic, meaning of unknown origin. Idiopathic growth hormone deficiency occurs, it seems, in about 1 in 3800 births.
GHD may also be hereditary, at least in some cases. About 3% of children with GHD have brothers or sisters who also have the disorder. In a very few families one of the parents is affected. The deficiency is two to three times more common in boys than in girls, for reasons quite unknown.
Children with GHD are small with normal skeletal proportions, facial appearance and intelligence. They tend to be overweight (this reduces during GH treatment) and they often have a delayed bone age. The diagnosis is confirmed by measuring the level of growth hormone production in response to a stimulation test, which normally requires a morning in hospital. The deficiency may be of growth hormone only, although other pituitary hormones may also be affected (MPHD).
| The associated hormone deficiencies are : | |
|---|---|
| 1. | thyroid-stimulating hormone (TSH) |
| 2. | the gonadatrophins – follicle stimulating hormone (FSH) and lutenising hormone (LH) |
| 3. | adrenal-stimulating hormone (ACTH) is much less frequently involved, but the deficiency of the hormone is extremely important to detect. |
If there is a deficiency of TSH, thyroxine is given, and if gonadotrophin deficiency becomes apparent at the time of puberty (which is usually late in growth hormone deficient children), the sex hormones have also to be given and treatment can initiate sexual maturation. Very occasionally antibodies develop to the injected growth hormone treatment and cancel out the effects of treatment but this is extremely rare with more modern biosynthetic human growth hormones; otherwise side-effects are unusual.
Causes of Growth Disorders
GROWTH ASSESSMENT / GROWTH DISORDERS
| Measure Every Child | |
|---|---|
| Weight : | birth 2, 4, 6, 8, 12, 16 weeks, 6-8 months, 1 year. |
| Length : | 10 days and 3 monthly up to year 1. |
| Height : | Yearly from 18 months, school entry and routine checks at school. |
| Head Circumference : | 36 hours, 10 days and 8 weeks and as indicated. |
If there is any concern about growth, measurements should be taken more frequently.
Record child’s measurement and plot on growth charts
| Measure real father and mother and calculate / plot mid parental centile [MPC] and target height range [TCR} | ||
|---|---|---|
| Is this child small/tall but appropriate for parental heights? | Yes | Normal short/tall stature |
| Is child inappropriately short/tall for parental heights? | Yes | Refer to Paed Endocrinologist |
| Is child growing at an inappropriate growth rate? | ||
Possible Diagnosis
| Short & Tall Stature | |
|---|---|
| Small for chronological age | GROWTH DELAY |
| Abnormal karyo type | CHROMOSOME ABNORMALITIES • Turner Syndrome • Down’s Syndrome |
| Low brithweight, thin, dysmorphic, possible asymmetry | INTRAUTERINE GROWTH RETARDATION (IUGR) • Including Russel Silver syndrome |
| Dysmorphic, cardiac problems | NOONAN SYNDROME |
| Abnormal hypopituitary function | ENDOCRINE DISORDERS • Growth hormone insufficiency • Panhypopituitarism • Hypothyroidism • Cushing's Syndrome • Premature sexual Maturation • Environmental growth failure |
| Dysmorphic | BONE DYSPLASIAS • Achondroplasia • Hypochondroplasia |
| Chronic ill health | CHRONIC DISEASES • Congenital heart disease • Renal failure • Coeliac/Crohn’s disease • Cystic Fibrosis • Asthma / eczema |
| Inappropriate tall stature | SYNDROMES • Marfan • Sotos • Klinefelter’s ENDOCRINE • Precocious puberty |
NORMAL GENETIC SHORT/TALL STATURE
 All children who are considered short/tall should be assessed for their MPC and TCR (see page 5). If their height is within normal limits for their parents and they are growing at a normal rate, they are normal, whatever their position within the population standards.
All children who are considered short/tall should be assessed for their MPC and TCR (see page 5). If their height is within normal limits for their parents and they are growing at a normal rate, they are normal, whatever their position within the population standards.
There is no effective treatment for genetic short stature. The availability of biosynthetic growth hormone has allowed increased interest in the use of this substance for the treatment of children who are very short. This is still in the stage of clinical trials but available evidence suggests that final stature will not be altered significantly. While it is clear that even in children with normal growth hormone secretion, a short-term acceleration in growth may be achieved during growth hormone therapy, there is no certainty at this time that the long-term final height prognosis is altered. Further careful studies, extending over a number of years, will be necessary to show this. However, in the USA, there is a much more liberal treatment regimen for children with genetic short stature. Although this probably represents a very heterogeneous group of children, growth hormone is now licensed for use in this indication.
CONSTITUTIONAL DELAY/ADVANCEMENT OF GROWTH AND PUBERTY
Constitutional delay of growth in puberty (CGDP) frequently causes concern and seems to be more prevalent in boys than girls. It is often first noticed when the boy seems to have stopped growing, has younger siblings catching up or even being taller than him, or has classmates leaving hi behind. Growth delay of up to two years is not uncommon and a small number of children are delayed three, or even four years. Frequently one of the parents, an aunt or an uncle, brother or sister, will have had growth delay. A mother will often be able to establish that she was 15 or more years old at menarche instead of the more usual 12 to 14 years : it may be more difficult to establish a father’s pubertal delay owing to the lack of a fixed event such as menarche.
Once growth delay has been established any boy or girl can be absolutely reassured that puberty occurs in the end and that they will develop quite normally in every way. They can be reassured with a full demonstration of facts, figures, charts and predictions. Children find the information that they are simply taking after their mothers or fathers reassuring if not particularly welcome. What reassurance does not do is remove the very real physical handicap associated with being small and, worse, remaining pre-pubertal with a peer group of adolescents.
Safety Profile of GH
GROWTH ASSESSMENT / GROWTH DISORDERS
(A GUIDE FOR PARENTS AND PATIENTS)
GP Promotes the growth of muscle and bones, while the shift of lipid metabolism tends to be in the opposite direction. So, although a child’s appetite often increases, body fat may decrease with GH treatment. This is because GH contributes to the breakdown of fat at the same time the child is using more calories for growth of bone, muscle and other supporting tissues.
A small percentage of children receiving GH develop a low level of weak antibodies to the medication. This means that the body recognizes the GH as a foreign protein. These antibodies are rarely of any significance, although a high level of strong antibodies can block the action of GH. if this occurs, treatment is stopped temporarily and restarted with a different brand of GH.
In some children, the need for GH therapy results from treatment they received for leukemia or a brain tumor. Based on information collected from around the world, it does not appear that GH treatment increases the risk of relapse or recurrence in these children; relapse rates are similar in children who have received GH and those who have not GH has not been associated with an increased risk of cancer in childhood.
Several cases of benign intracranial hypertension (IC) have been reported in children starting GH starting treatment. IC results from increased pressure in the brain and can produce symptoms such as headaches, visual changes, nausea and vomiting. Most reported cases have occurred within the first 8 weeks of treatment and resolved after stopping GH or reducing the does.
Psychological effects of GH:
The overall psychological effects of GH therapy are positive; an increased growth rate, more mature appearance and the hope for an adult height within the normal range are viewed as positive by both parents and children. Even seemingly trivial milestones, such as being able to reach a light switch, give beneficial reinforcement.
Some children expect too much from GH - they think they will grow overnight or become the tallest in their class. When these expectations are not met, the child may feel dissapointed, depressed, or even guilty. The response to GH is individualized and depends on many factors.
Although self-esteem and body image may improve as the child begins to catch up to peers in size, GH does not cure behavior problems or remove all the child’s stress.
It’s not unusual for young children to regress temporarily after starting on GH (bed-wetting, thumb-sucking, irritability); older children may complain of headaches, stomachaches, or fatigue.
Safety profile of GH:
Indication for Growth Hormone
GROWTH ASSESSMENT / GROWTH DISORDERS
(A GUIDE FOR PARENTS AND PATIENTS)
Sotos syndrome or Cerebral Gigantism
Diagnosis : From around 2-4 years of age. Tall stature and dysmorphic features.
 Sotos syndrome, or gigantism, usually presents in early childhood. The physical characteristics are tall stature, large hands and feet and poor circulation. There may also be special educational needs. Bone age is often advanced and puberty usually occurs early so excessive tall stature may not be a feature of adulthood.
Sotos syndrome, or gigantism, usually presents in early childhood. The physical characteristics are tall stature, large hands and feet and poor circulation. There may also be special educational needs. Bone age is often advanced and puberty usually occurs early so excessive tall stature may not be a feature of adulthood.
Growth Harmone and its effects:
A doctor’s recommendation to begin a child on growth hormone (GH) is based on consideration of many factors, including a complete evaluation of the child’s growth pattern, general health, medical and family history, and results of laboratory tests. Parents may have many questions when they are considering a doctor’s recommendation to start their child on GH. Perhaps most importantly, parents well want to understand the potential benefits and risks of GH treatment. The pediatric endocrinologist who is evaluating the child is the best person to answer these questions. This fact sheet about the possible effects of GH is intended to serve as a brief overview for parents, not as a substitute for a thorough discussion with the child’s health care team. Much of the information contained here about the physical effects of GH is based on the official statement of the European Society of Pediatric Endocrinology cocerning the safety and toxicity of GH, which has also been endorsed by the Lawson Wilkins Pediatric Endocrine Society in the United States.
Physical effects of GH:
GH deficient children will grown faster, often 2 to 3 times their pre-treatment growth rate during the first year of therapy. This increased (“catch-up”) rate wanes over time, but they should continue to grow at a normal rate while receiving therapy. GH deficient children who respond well to GH will be taller as adults than they would have been if not treated.
Indications for Growth Hormone
FDA approved indications
• GH deficiency(1985)
• Turner syndrome (1995)
• Chronic renal insufficiency – pretransplantation and post transplant (1995)
• Children born SGA who have not shown evidence of catch-up growth by 2 years of age (2001)
• Prader Willi syndrome with short stature( 2000)
• Idiopathic short stature >2. SD below the mean in height and who are unlikely to catch up in height (2003)
• Adult Growth Hormone Deficiency
• SHOX Deficiency 2006
• Noonan syndrome 2007
Other indications:
• HIV Wasting
• Cystic fibrosis
• X-linked hypophosphatemic rickets
• Precocious puberty
• Chronic glucorticoid use
• Thallasemia with short stature
• Trisomy syndrome
• Severe Burns
• IVF Spermatogensis
• Anti ageing
